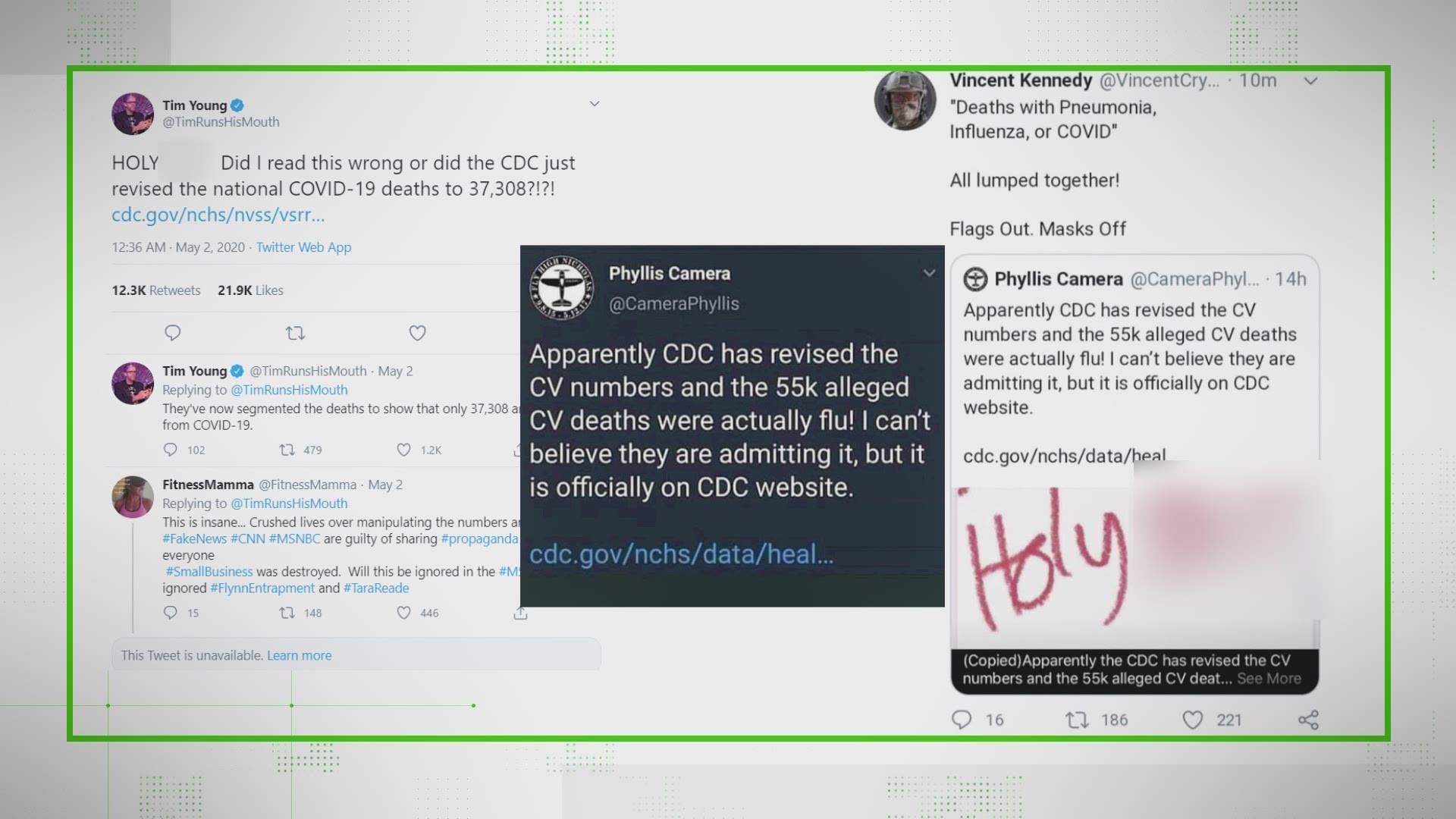
When the CARES Act passed, Twitter erupted with people who zeroed in on an emergency provision allowing hospitals to charge Medicare 20% more to treat COVID-19 patients. Critics saw it as a money grab and an enticement to overcount coronavirus cases.
THE QUESTION
Under the CARES Act, hospitals can add 20% to their fee for treating a COVID-19 patient on Medicare. Doesn’t this give hospitals an incentive to inflate the number of COVID-19 patients they treat?
THE ANSWER
No. In addition to undergoing audits, hospitals and providers face harsh repercussions if they cheat, according to federal law, and experts.
WHAT WE FOUND
First, the 20% add-on fee doesn’t mean the hospital is really making an extra 20% on every COVID-19 patient. It’s complicated, but essentially Medicare pays a hospital based on a diagnosis code assigned to a patient upon discharge. Medicare pays a flat rate on that diagnosis, but in reality the hospital may spend more or it may spend less to treat a specific patient.
So why an additional 20% in the CARES Act, a figure first proposed as 15%?
Karyn Schwartz, senior fellow and an expert in hospital reimbursement at Kaiser Family Foundation, said that hospitals, especially in New York and New Orleans, have faced unexpected expenses from the flood of COVID-19 patients. Among the extra costs, she said, were acquiring ventilators, setting up temporary structures to house patients and buying protective equipment for staff.
Hospitals also postponed elective surgeries, a key source of income, and some have furloughed or laid off workers as a result, said an American Hospital Association spokesman. Elective surgeries – meaning those scheduled ahead of time, whether minor or serious – included those for cancer patients and others who might need an ICU bed or a respirator.
As for a hospital inflating the number of COVID-19 patients for the Medicare add-on fee, there are measures to catch that, said Katherine Harris of the Health and Human Services Office of the Inspector General, the financial watchdog over Medicare.


“COVID-19 may be new, but inappropriate billing to boost profit is a very old story,” she said. Data analyses, done when claims are submitted, detect “upcoding” and unusual billing patterns, she said.
Hospitals also file an annual Medicare Cost Report, which is examined by Medicare auditors, whose work then faces an additional review.
Tipsters to the OIG fraud hotline also spark audits. And whistleblowers have an incentive to report fraud; they can receive 10% of recovered funds.
RELATED: VERIFY: What is remdesivir?
When suspicions arise, Medicare and OIG investigators swoop in for a harder look at the numbers. “If a Medicare provider inaccurately bills for services provided based on a beneficiary’s diagnosis, then CMS can recoup the payment and/or the provider can be disenrolled from the Medicare program,” a Centers for Medicare and Medicaid Services spokesman said.
Violators risk prison time. Depending on the circumstances, the punishment for defrauding Medicare ranges from five to 30 years, the Department of Justice says.
Something you’d like VERIFIED? Click here to submit your story.