(CNN) — Two separate outbreaks this month of the rare but deadly toxin botulism have focused attention on this potentially fatal illness, which usually strikes about 150 people a year, mostly infants.
In Sacramento, California, one person died and nine others were hospitalized after eating gas station nacho cheese contaminated with the toxin, likely from improper heating and storage.
Another death from botulism occurred in nearby Napa County earlier in May, according to county public health director Dr. Karen Relucio. “We are suspicious that canned goods might be the source, but we have not yet fully identified the food,” she said.
What is botulism?
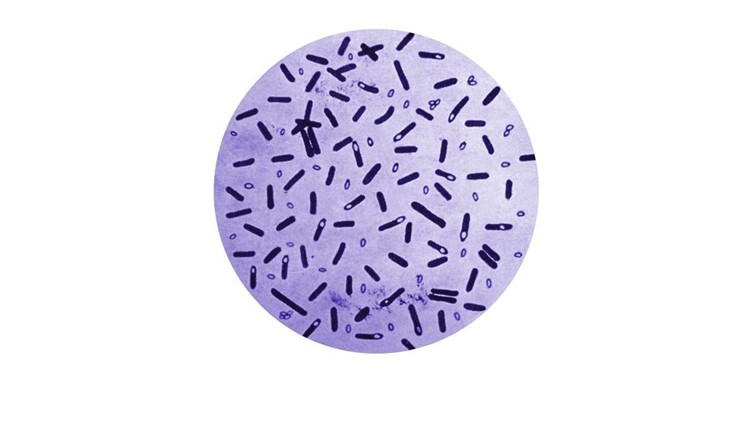
Botulism is a paralyzing nerve toxin, considered to be one of the most potent and lethal substances in the world. It’s produced by the bacterium Clostridium botulinum and sometimes by strains of Clostridium butyricum and Clostridium baratii. The rod-shaped bacteria are commonly found in soil and sediments from lakes, rivers and oceans. They thrive in low-oxygen conditions, such as canned foods, deep wounds and the intestinal tract, but when threatened form protective spores with a hard coating that allows the bacteria to survive for years.
The danger is not from the spores themselves but what they produce while germinating. As the C. botulinum bacteria grow, they create eight types of neurotoxins that are so deadly, even microscopic amounts can kill.
This deadly nerve toxin is also the source of Botox, a leading cosmetic solution for wrinkles as well as medical conditions such as migraines and excessive sweating, known as hyperhidrosis. Injecting minute, highly diluted amounts of the toxin into a muscle blocks the nerve signals that tell that muscle to contract. That temporarily weakens the muscle, thus smoothing the wrinkle or the pain the contraction causes.
What are the symptoms of botulism?
Because botulism toxin paralyzes muscles, early and classic signs of the illness are drooping eyelids and blurred or double vision, dry mouth, slurred speech and difficulty swallowing. If left untreated, greater paralysis of muscles of the arms, legs and trunk of the body will occur, affecting the ability to breathe.
Babies infected with botulism will be poor feeders and seem lethargic, with a weak cry and poor muscle tone. They can also be constipated.
Botulism does not cause fever, and those affected are usually alert and aware of their surroundings.
How is botulism treated?
Unless there is a clear cause, such as obviously contaminated food, doctors will first rule out other diseases that can mimic the symptoms of botulism, such as stroke and Lyme disease.
Once botulism is confirmed, it can be treated with an antitoxin and, in some cases, antibiotics. If the antitoxin is given before paralysis is complete, it helps shorten recovery, which requires the regrowth of motor nerve endings. The patient can be hospitalized for supportive treatment, such as a ventilator, for weeks or months until the paralysis improves. In some cases, muscle weakness and shortness of breath can last years.
Other treatment depends on the kind of botulism, of which there are five main types:
Infant botulism
In 2001, there were 169 cases of botulism in the United States. Among those, the vast majority — 112 cases — were in infants. In 2015, 141 of the 199 confirmed cases of botulism in the US were in infants.
Although infants can be infected by swallowing contaminated soil, feeding an infant under the age of 1 honey or corn syrup is the main culprit. Their immature digestive systems cannot move C. botulinum spores through their gut quickly enough to keep the spores from germinating.
For the same reason, babies who have less than one stool a day for more than two months are also at risk. The illness is most common in those between 6 weeks and 6 months.
If the illness caught and treated early, most infants make a full recovery. However, antibiotics are not used in children of this age, as killing the toxin in their intestines can trigger the release of additional antitoxins. Instead, vomiting and enemas are typically used to get rid of undigested food in the gut.
Food-borne botulism
C. botulinum spores are commonly found on the surfaces of seafood and most fruits and vegetables. Due to today’s manufacturing methods, it’s rare for store-bought foods to be contaminated with botulism. The common culprit in much food-borne illness is homemade food that has not been properly canned or fermented.
One of the largest recent outbreaks occurred in April 2015, after a church potluck meal in Ohio. Twenty-nine people were infected with botulism, likely after eating potato salad made with home-canned potatoes that were made with a boiling water canner, which doesn’t kill C. botulinum spores, instead of a pressure canner.
Anyone canning food at home should carefully read materials on which fruits and vegetables need special canning methods and follow directions closely.
And always inspect any store-bought or home-canned food containers closely. Look for swelling, such as bulges, damage or cracks, and leaking. If you see any, don’t open, just toss.
If the food smells or looks bad or the container squirts or foams when opened, throw it out immediately and use bleach to wipe up any spills.
According to the Centers for Disease Control and Prevention, “You cannot see, smell, or taste botulinum toxin — but taking even a small taste of food containing this toxin can be deadly.”
Symptoms of food-borne botulism normally begin 18 to 36 hours after ingestion, but they can happen as early as six hours or as late as 10 days after eating contaminated food.
Treatment often includes trying to remove contaminated food from the intestinal tract by inducing vomiting or using enemas.
Wound botulism
If the spores find their way into the body via a wound, especially a deep one, the low-oxygen environment will encourage their growth. People who inject heroin and other drugs are at high risk for this type of illness, but it has also been known to occur after serious injuries from car or motorcycle accidents, and even after surgery.
Wounds containing botulism are normally surgically cleaned to remove the source, and the patient will probably be given a round of antibiotics.
Adult intestinal toxemia
This is a very rare type of botulism in which the spores get into an adult’s intestinal tract. It’s similar to infant botulism, but science isn’t very clear on how the spores get into the adult gut. It’s thought that people with gastrointestinal health conditions may be more susceptible.
Latrogenic botulism
This type of botulism occurs when too much of the cosmetic form, Botox, is injected into a muscle. Although rare, it can happen when people use knockoff versions of the drug, for example, at “Botox parties,” that may not be as carefully prepared as the commercial version. Or when there is a terrible mistake.
In 2004, four people were hospitalized after receiving injections of Botox labled “For research purposes only. Not for human use.” According to a case review in the Journal of the American Medical Association, “the 4 case-patients in this cluster may have each been exposed to up to 8 million mLD50, which is 2857 times the estimated human lethal dose by injection, of unlicensed botulinum toxin A due to a dilution error.”
The doctor who administered the injections pleaded guilty and was sentenced to three years in prison. The people responsible for the shipment also pleaded guilty to federal charges and were sentenced to prison and ordered to pay restitution.